A tool for more informed prescriptions.
Service Design
With MSD Merck Sharp & Dohme
Challenge
Help healthcare professionals to make more informed decisions when prescribing antibiotics, so as to contribute to a stronger control of antibiotic resistance.
Outcome
A validated solution that serves different types of healthcare professionals that are directly involved with the prescription of antibiotics.
- Client
- MSD Merck Sharp & Dohme
- Service
- Service Design
- Location
- Portugal
- Duration
- 10 weeks
- fields
- Research, Strategy, Prototyping, Validation, UX, UI
- team
- Tiago Nunes,
João Joaquim
,Raquel Félix
,Mónica Pacheco
,Guilherme Rua
Context
In a hospital environment, antibiotics are often prescribed lightly and with little consideration for antibiotic resistance. A recent World Health Organization report called for urgent action to avert the antimicrobial resistance (AMR) crisis, which is predicted to cause 10 million deaths each year by 2050.
The prescription of antibiotics has become commonplace. How can we develop a solution that helps doctors, nurses, pharmacists, and other healthcare professionals to be more mindful when prescribing antibiotics and, ultimately, to help counteract the growing epidemic of antibiotic resistance?
As a way to make more informed decisions, health professionals need to be informed about the antibiotic consumption and the ecology of their service and hospital, thus contributing to a better control of antibiotic resistance.
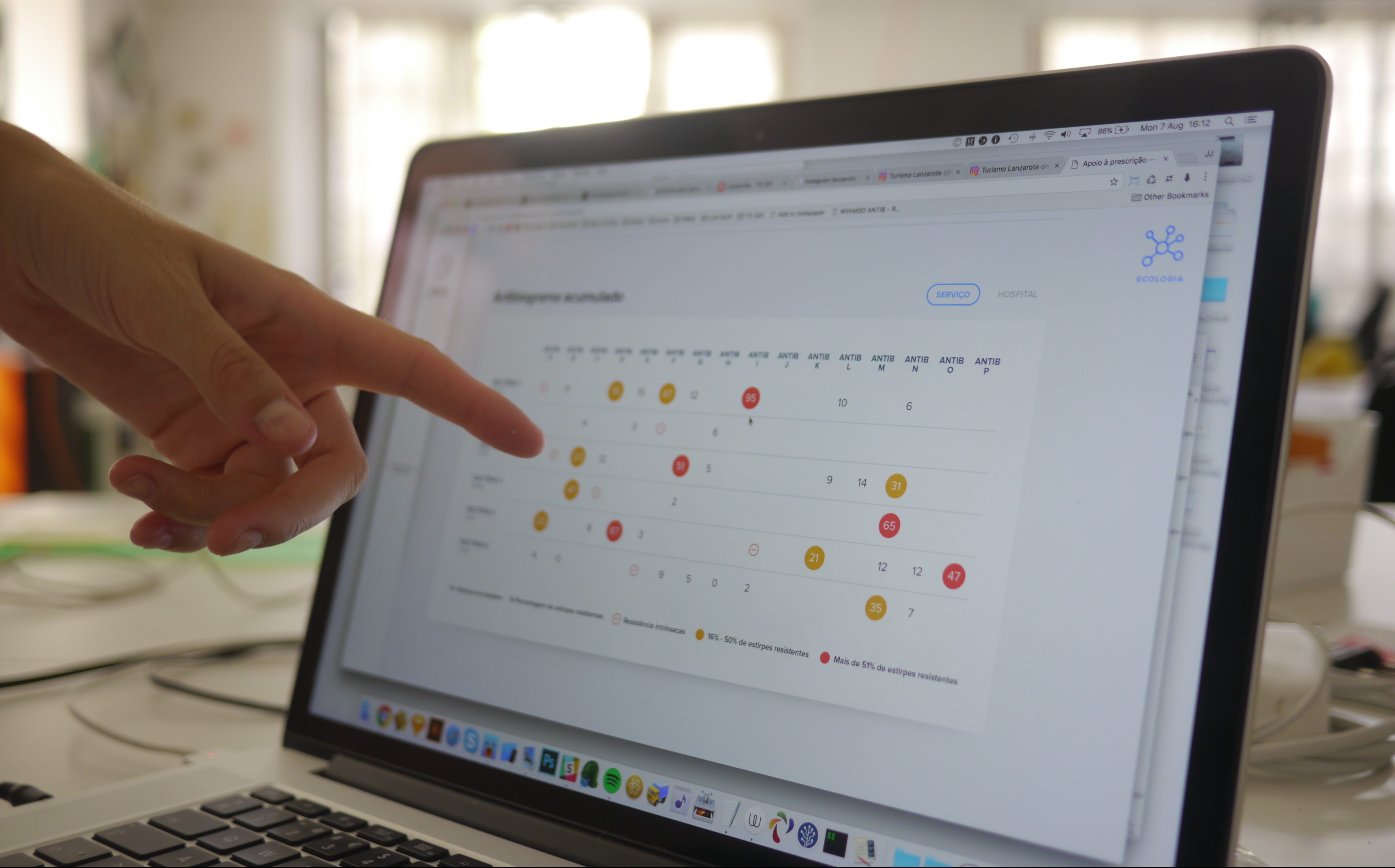
One of the solutions lies in creating antibiograms. Antibiograms allow hospitals and health professionals to identify how susceptible strains of pathogens are to a number of antibiotics, and are becoming an increasingly popular solution among the medical community and infection control teams. However, they are time-consuming to create and to maintain.
Some national programs (PPCIRA) and hospitals have already developed a few solutions, however, results have been far from effective. MSD called us in to create a more tangible and impactful solution.
Our role
01
Create a solution where the long-term impact of prescribing antibiotics is visible and measurable.
02
Improve the way information about hospital ecology is shared and read.

RESEARCH
Our biggest challenge was to simplify a very complex matter. Health professionals are generally very focused on the patient and, therefore, mostly concerned about the short-term impact. However, antibiotic resistance isn’t exactly written on people’s forehead, which makes it harder to be aware of any long-term impacts.
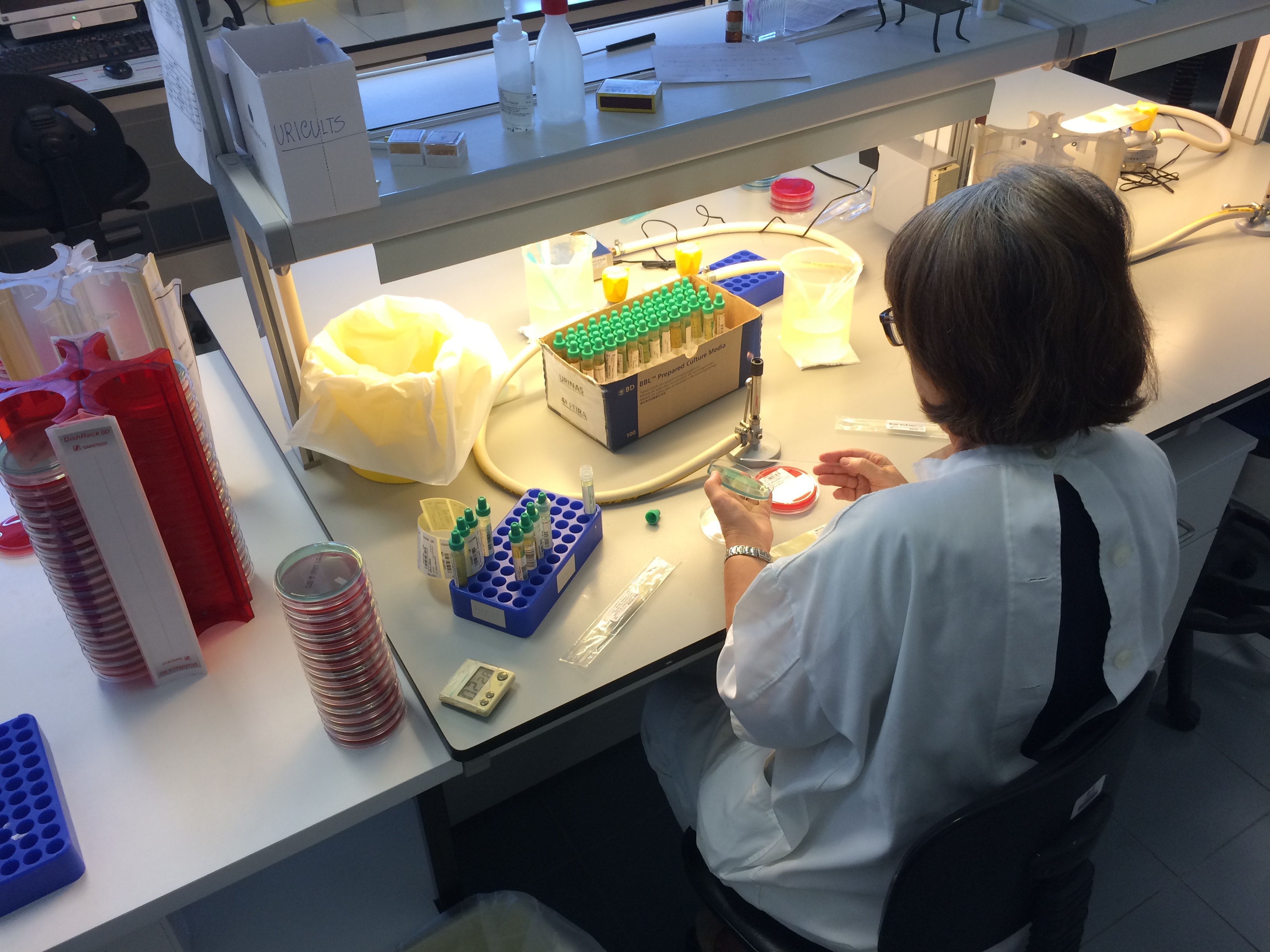
Through several interviews, surveys, and benchmarking, we were able to understand the complexity of this topic, particularly the reasons that are interfering with more informed prescriptions.
To better understand the way an antibiogram works and how it is perceived, we mapped the pains, the process, and the tools associated with it. The overall feeling is that it is too simplistic, linear, and generic. The fact that antibiograms aren’t mandatory also tarnishes their reputation and holds back their distribution.
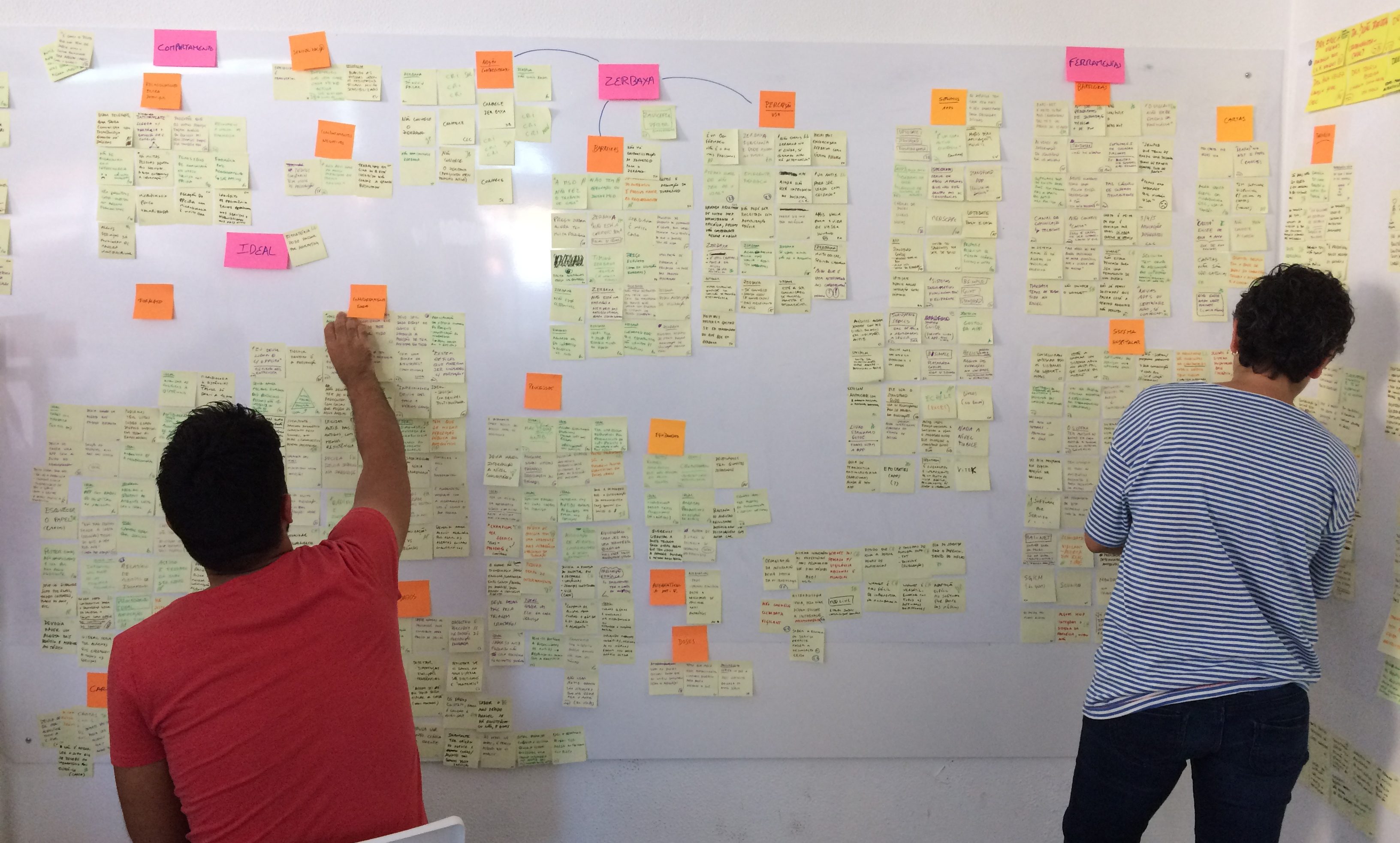
The subjects of this project were the solution’s future end-users. Therefore, our strategy depended on a full understanding of who these professionals are and what they think. From the interviews phase to the ideation phase, we fostered a close relationship with these healthcare professionals through co-creation sessions and constant iteration.
5214
Hands washed
27
Interviews
20
Hours of observation
10
Known bacteria
5
Hospitals visited
Findings
After surveying several different types of healthcare professionals, more than half of respondents admitted that they were unaware of an antibiogram being used in the hospital they work in. And, those who were aware mentioned that the antibiogram becomes irrelevant because it is not updated regularly. We also found that:
- respondents prescribed two or more antibiotics a day
- hospitals don’t provide sufficient information about bacterial resistance
We also identified how much culture impacts and reinforces this problem. A large portion of the population has the false perception that doctors who don’t prescribe antibiotics are bad professionals. Moreover, even though selling antibiotics over-the-counter is forbidden, it hasn’t stopped pharmacists from doing so without a prescription. The frequent use of antibiotics had become trivial to doctors, pharmacists, and patients alike.
The lack of a decent technical solution, combined with the absence of prescription guidelines, has prompted each healthcare service to act independently. How can we bring these professionals together and what could a one-stop-shop solution look like?


Prototyping
When coming up with a prototype, we were inspired by a completely different and unexpected industry that also deals with undesired resistances: Agronomy. By comparing bacteria to weeds and herbicide to antibiotics, we were able to create an analogy that paved the way to create our final prototype.
Due to the high quality of solutions that resulted from the co-creation workshop, we were able to quickly formulate a prototype, test it, and improve it along the validation process. We were able to create three versions in the space of two weeks, and produce a hi-fi final prototype.
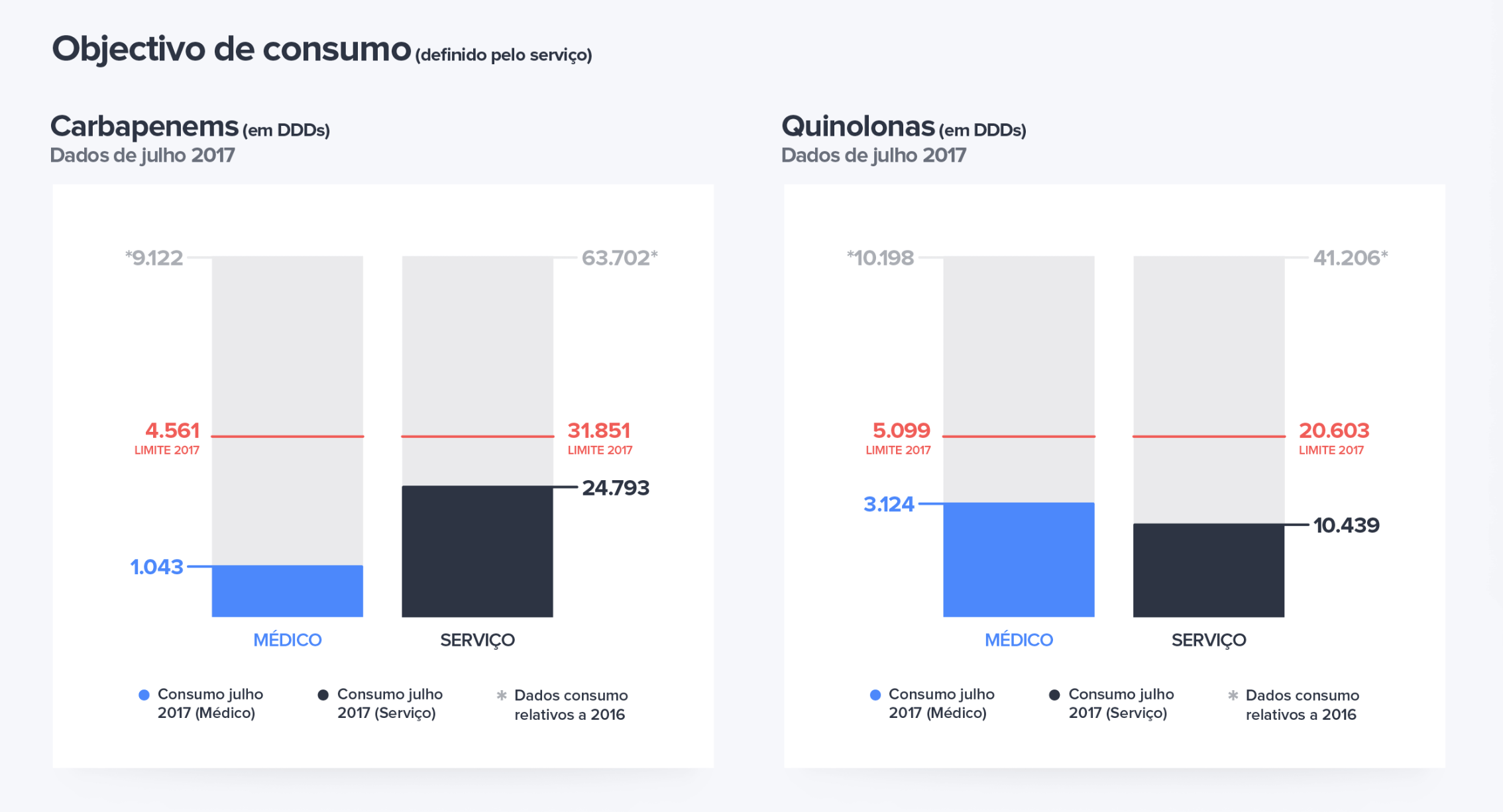
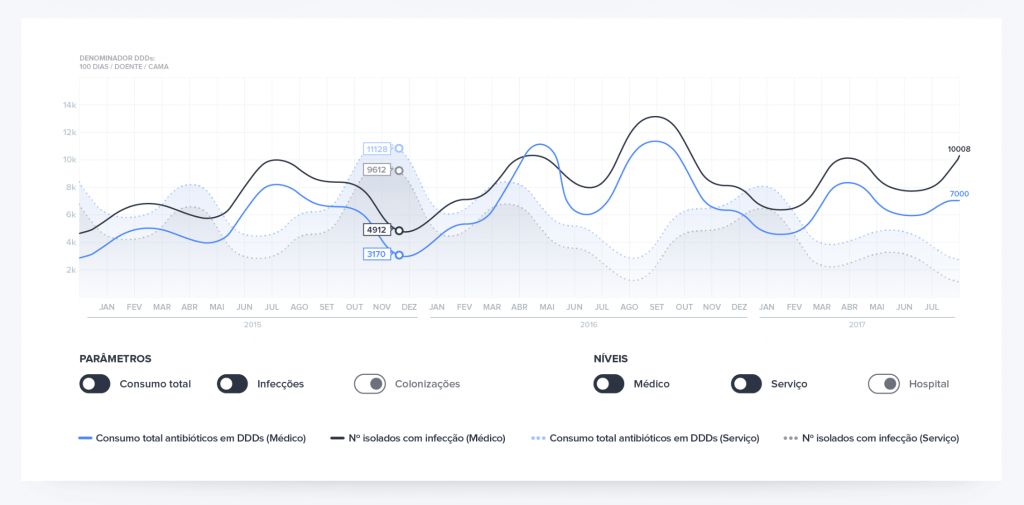
Across two dashboards, our prototype includes:
- an intuitive graph comparing the consumption of antibiotics in absolute values
- a simple chart revealing five of the most commonly prescribed antibiotics to easily identify patterns
- a “red flag” graph pinpointing which antibiotics are being prescribed in greater number, and whose prescription should be immediately decreased
- a cumulative antibiogram that immediately shows all the information about the hospital or service’s ecology
Results
Our prototype was extremely well received, with:
- several services showing interest in beta-testing
- everyone underlining the importance of having a graphical representation of current use and goals
- all professionals considering the filtered antibiogram to be pertinent

88% of the healthcare professionals we showed the prototype to said they would use this solution every day.
By aggregating data from different stakeholders (hospital pharmacy, patient information, antibiotic and resistance data) this solution could soon become even more personalised, perhaps even to the doctor-patient level, contributing to a proper use of antibiotics — even turning the antimicrobial resistance trend around.








